5 Common Denial Mistakes Nurses & Providers Make—And How to Fix Them Fast
Every denial started as a preventable problem somewhere. Your role isn't just to provide excellent patient care - it's also to ensure that care translates into successful reimbursement and covered services for your patients.
JL Love
9/25/20253 min read
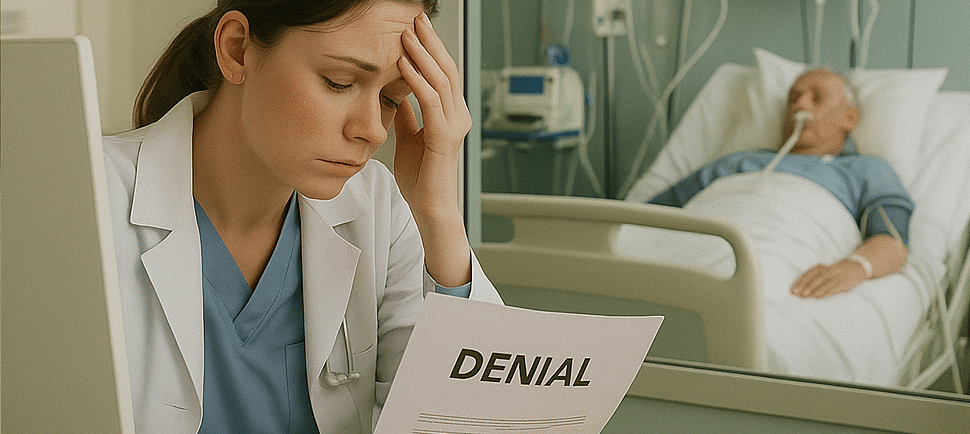
Insurance claim denials are frustrating, time-intensive, and expensive. But here's the thing: many denials are completely preventable. The problem isn't that the system is broken (though it sometimes feels that way)—it's that we're making simple, fixable mistakes that trigger automatic denials.
Let me share the five most common denial mistakes I see nurses and healthcare providers make every single day, plus a quick preview of how to fix them.
The Insurance Card Shuffle
The Problem: Patient has new insurance but keeps presenting an old card. Or doesn’t have a card at all.
Why It Gets Denied: Coverage lapses, wrong policy numbers, or verification not updated. More insurance companies are doing away with physical cards and opting for e-cards but for older, analog patients they may not know how to access it.
The Fix: Ask patients when they last used their insurance successfully. Also check for any secondary coverage. Take advantage of all new e-verification methods for your top payers to validate coverage.
The Authorization Time Bomb
The Problem: Many procedures require prior authorization but it isn’t always obtained. Authorizations expire, wrong codes are used, or requirements are missed.
Why It Gets Denied: Insurance requirements change often, and what was routine coverage six months ago might now require pre-approval. Or there have been changes in the treatment plan and the prior authorization is no longer valid.
The Fix: Create a system that always validates authorization status. All charting should support the medical necessity of any procedure in the event an appeal is required.
Documentation Disconnect
The Problem: The use of vague terms like “rule out,” “likely,” or “possible" and not using confirmed billable diagnosis codes in documentation.
Why It Gets Denied: A red flag to insurance companies- choosing a higher level of service without the proper documentation to support it.
The Fix: Use confirmed diagnoses or patient symptoms if a condition is uncertain when charting. CPT/HCPCS codes should always align with the diagnoses that justify medical necessity. For example, billing an EKG without a related diagnosis (like chest pain or arrhythmia) risks denial.
Out of Sight- Out of Time
The Problem: Waiting until the end of the month (or longer) to submit claims, missing crucial filing deadlines.
Why It Gets Denied: Every insurance company has strict filing deadlines. Miss the window, and even perfect claims get denied for being "untimely."
The Fix: Implement a "24-48-7" filing system that prevents timing-related denials. It looks like this:
Day 1 (Visit scheduled/completed) → Verify insurance & pre-auth done.
Day 2-3 (Within 48h) → Provider closes chart, coder applies CPT/ICD codes.
Day 7 (End of week) → Claim out the door, confirmation in EHR/billing software.
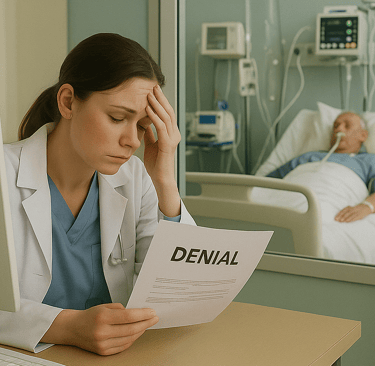
The Real Cost of These Mistakes
These aren't just minor administrative hiccups. Denial mistakes cost the average healthcare practice:
2-4 hours per day in rework and appeals
15-20% of potential revenue in lost or delayed payments
Increased stress and job dissatisfaction for nursing staff
Patient satisfaction issues when services are delayed
Don't Let Another Denial Slip Through
Consider this: practices complete an average of 43 prior authorization requests per physician each week, and physicians and their staff spend 12 hours per week completing these requests (AMA, 2024). When those requests get denied, the administrative burden multiplies exponentially. But when we get it right the first time, everyone wins. The best denial is the one that never happens.
About the Author: JL Love is a nurse with over 35 years' experience spanning emergency medicine, critical care, case management, and utilization review. Having led large clinical teams and written hundreds of appeals, she has developed a reputation for turning complex denial challenges into practical, results-driven strategies.
Get your copy of "From Denied to Approved: Templates, Strategies and Metrics for Appeal Success" on Amazon today →
Available in both digital and print formats.