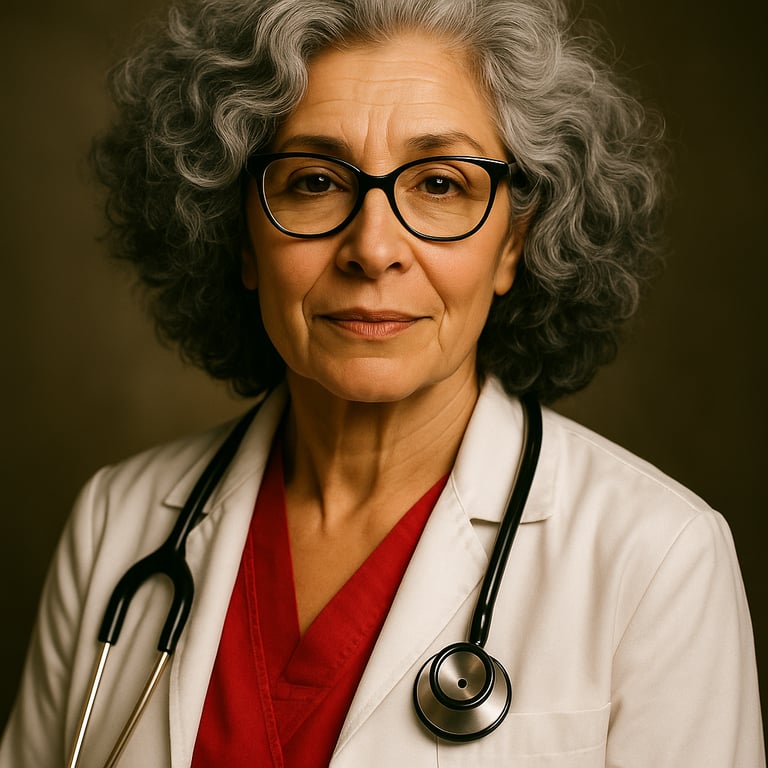
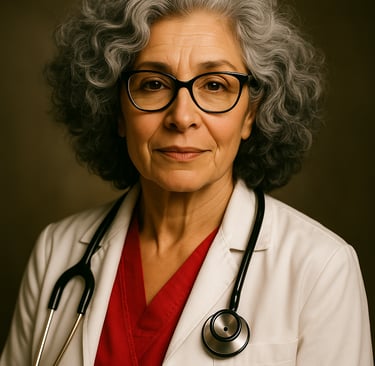
The Wisdom We're Losing: Why Ageism in Nursing Hurts Everyone
Addresses the important issue of ageism in nursing while highlighting the crucial mentoring role that experienced nurses play. The post challenges the misguided practice of cancelling out older nurses and emphasizes how this hurts everyone involved - patients, new nurses, healthcare institutions, and the profession as a whole.
9/25/20254 min read
When a local hospital recently offered buyout packages to all employees 60 years and older, it sent a clear message: your experience has an expiration date. At 60, these nurses weren't being celebrated for their decades of knowledge—they were being shown the door. This troubling trend reflects a broader issue plaguing healthcare: ageism in nursing that's not just unfair, it's dangerous for patient care and the profession itself.
The False Promise of "Fresh Blood"
Healthcare administrators often justify pushing out older nurses with phrases like "bringing in fresh perspectives" or "modernizing our workforce." But what they're really doing is discarding irreplaceable institutional knowledge and breaking the crucial chain of mentorship that has sustained nursing for generations.
Sometimes this ageism isn't overt—it's embedded in the very design of "modern" healthcare environments. Consider one hospital's recent restructuring: out went the traditional cafeteria with human cashiers who accepted cash and served comfort foods like French fries and fried chicken. In came a "futuristic" space with cashless payment systems, automated ordering, healthier menu options, and seating areas filled with couches, bean bags, and rolling tables. While well-intentioned, the message to experienced staff was clear: "This was made for 20-year-olds." Nurses with decades of experience suddenly felt out of place in their own workplace—not because they couldn't adapt, but because no one considered their needs when designing these "improvements."
Consider what a nurse with 35 years of experience brings to the bedside. They've seen medical trends come and go, witnessed the evolution of treatments, and developed an intuitive sense for patient assessment that can't be taught in nursing school. They've navigated countless emergencies, comforted thousands of families, and accumulated wisdom that technology simply cannot replace.
The Mentorship Gap
Perhaps most critically, experienced nurses serve as the bridge between textbook knowledge and real-world practice. They're the ones who teach new graduates:
How to trust their instincts when something doesn't feel right about a patient
The art of therapeutic communication with difficult families
How to prioritize care when everything seems urgent
The subtle signs that often precede medical emergencies
How to advocate effectively for patients within complex healthcare systems
When we push out older nurses, we're not just losing individual expertise—we're breaking the mentorship chain that transforms nervous new graduates into confident, competent nurses. Young nurses need these experienced mentors to develop clinical judgment, emotional resilience, and professional identity.
The Reality Check: 60 Is Not Old
Let's be honest: 60 years old in 2024 is not what 60 looked like decades ago. Ads today promote older women in all of their gray-haired, active, strong-willed glory. Today's 60-year-old nurses are often at the peak of their professional capabilities. They have the energy to work full shifts, the wisdom to handle complex situations, and the passion that comes from choosing nursing as a calling, not just a career.
Many of these nurses have adapted beautifully to technological advances, electronic health records, and evolving protocols. They've proven their resilience through pandemic response, staffing shortages, and constant healthcare changes. To assume they're ready for retirement simply based on age is both discriminatory and short-sighted.
The Cost of Ageism
When hospitals systematically encourage older nurses to leave, everyone loses:
Patients lose access to nurses with deep clinical experience and refined assessment skills that can mean the difference between catching a complication early or missing it entirely.
New nurses lose mentors who could guide them through the challenging transition from student to professional, leading to higher turnover rates and longer learning curves.
Healthcare institutions lose valuable knowledge, continuity of care, and the stability that experienced staff provides during challenging times.
The profession loses its memory, its standards, and its sense of continuity across generations.
A Better Way Forward
Instead of pushing out experienced nurses, healthcare organizations should be creating environments where multi-generational teams thrive:
Formal mentorship programs that pair experienced nurses with new graduates, creating structured opportunities for knowledge transfer.
Flexible scheduling options that accommodate the needs of older nurses while utilizing their expertise during critical situations.
Recognition of expertise through roles like charge nurse, educator, or clinical specialist that leverage years of experience.
Knowledge preservation initiatives that document and share the wisdom of veteran nurses before they retire.
Age-inclusive cultures that value both innovation and experience, recognizing that the best healthcare teams include nurses from multiple generations.
The Bottom Line
Every time we lose an experienced nurse to ageism, we lose a piece of nursing's collective wisdom. We lose mentors who could shape the next generation of nurses. We lose advocates who understand both the art and science of nursing care.
At 60, nurses aren't too old—they're experienced. They're not outdated—they're seasoned. They're not ready to be put out to pasture—they're ready to pass on decades of knowledge to those who need it most.
The nursing profession faces critical shortages and high turnover rates among new graduates. The solution isn't to push out our most experienced nurses—it's to embrace the incredible resource they represent and create systems that honor both their contributions and their potential to guide the future of nursing.
Healthcare organizations that recognize this will find themselves with stronger teams, better patient outcomes, and a culture of learning that benefits everyone. Those that don't will continue to wonder why their new nurses struggle and their turnover rates remain high.
The choice is clear: we can either value the wisdom of experience or continue losing the mentors who make good nurses great. The future of nursing may well depend on which path we choose.